Extractions and Bone Grafts
What to expect during the tooth extraction process.
 When your dentist performs the extraction you should expect that you will feel a lot of pressure, here’s why.
When your dentist performs the extraction you should expect that you will feel a lot of pressure, here’s why.
The root portion of a tooth is firmly encased in bone (its socket) and it is tightly bound into place in this socket by a ligament. During the extraction process the dentist needs to expand the socket (widen and enlarge it) and separate the tooth from its ligament to a point where the tooth is loose and free to come out.
The bone of the jaw is compressible to some degree. That means if a dentist can apply firm pressure to a tooth, forcing it against one of the sides of its socket, the bone in that area will become compressed. The net result is that the socket becomes slightly enlarged. After repeated application of pressure to a tooth, from many different directions, the entire socket becomes larger. The ligament that holds the tooth in place will become detached from the tooth too. Finally at some point, enough space will have been created and the ligament separated from the tooth enough that the tooth will come out.
Dentists have a variety of tools they use to manipulate and apply pressure to teeth. Some of them are specialized pliers termed “extraction forceps.” Dentists also use levers that are called “elevators” (they look somewhat similar to small screwdrivers). Usually a dentist will use an elevator first. These tools are intended to wedge between the tooth and the bone surrounding it. The force the dentist applies to the elevator in turn places pressure on the tooth. This action on the tooth helps to expand its socket and separate its ligament. It’s somewhat common that a tooth can be extracted with just the use of an elevator.
Understanding the dentist’s use of extraction forceps is more straightforward. The dentist will grasp the tooth with the forceps and then firmly and deliberately rock the tooth back and forth. They will also rotate the tooth as much as it will. The combination of these tooth movements expands the tooth’s socket and separates its ligament.
Why you will feel pressure, yet no pain, during a tooth extraction.
The reason you will feel pressure during the tooth extraction process is because our bodies have different types of nerve fibers, each of which carry different types of sensations. Each of these different types of nerve fibers have different physical characteristics. The local anesthetic (“novocaine,” more actually usually lidocaine) that a dentist uses to “numb up” a tooth is very effective at inhibiting the function of nerve fibers that transmit pain sensations, but it doesn’t have as great an effect on the nerves that transmit pressure sensations.
So, expect to feel pressure during the tooth extraction process, even a whole lot of pressure, but don’t assume that this indicates that you will soon be feeling pain because it doesn’t. If you do find you feel pain (discomfort that has a sharpness to it) during the extraction process, you should let your dentist know so they can “numb you up” some more. But more anesthetic will not reduce the pressure sensation you are experiencing.
You might hear some extraction noises.
It is possible that during a tooth’s removal you will hear some of the noises associated with the extraction process. As an example, patients are sometimes concerned that they have heard a snap or breaking noise. In most cases the event that has produced this type of sound is just a minor issue, usually one of the tooth’s roots fracturing. Because this “complication” happens so frequently you can anticipate that your dentist has had plenty of experience in removing broken tooth roots.
Gum and bone tissue removal.
Gum and/or bone tissue may cover over or surround a tooth in a manner that makes it difficult for the dentist to view and/or access it. If so, the dentist will need to reflect back or remove this tissue.
Sectioning a tooth during an extraction.
Sometimes a tooth is so firmly anchored in its socket, or else the tooth’s roots are so curved, that the dentist can’t get the tooth’s socket expanded enough that it will come out. In this type of situation one of a dentist’s tricks is to cut the tooth into pieces and then remove each portion individually.
Don’t be alarmed if your dentist tells you that this technique is required. Sectioning teeth is very commonplace and can significantly reduce the amount of time and effort needed to remove a tooth.
Wisdom Teeth
Wisdom teeth, also known as third molars, are the last teeth to erupt in your mouth. This generally occurs between the ages of 17 and 25, a time of life that has been called the “Age of Wisdom.”
Anthropologists note that the rough diet of early humans resulted in the excessive wear of their teeth. Normal drifting of the teeth to compensate for this wear ensured that space was available for most wisdom teeth to erupt by adolescence. The modern diet, which is much softer, and the popularity of orthodontic tooth straightening procedures produce a fuller dental arch, which quite commonly doesn’t leave room for the wisdom teeth to erupt, thereby setting the stage for problems when the final four molars enter the mouth.
What is an Impacted Tooth?
Complications such as infection (fig. a) , damage to adjacent teeth (fig. b) and the formation of cysts (fig. c) may arise from impacted teeth.

(a) Infection

( b ) Crowding, damage

(c) Cyst
A tooth becomes impacted when there is a lack of space in the dental arch and its growth and eruption are prevented by overlying gum, bone or another tooth.
How Serious is an Impacted Tooth?
Impacted teeth can be painful and lead to infection.They may also crowd or damage adjacent teeth or roots.
More serious problems may occur if the sac surrounding the impacted tooth becomes filled with fluid and enlarges to form a cyst. As the cyst grows it may hollow out the jaw and permanently damage adjacent teeth, the surrounding bone and nerves. Rarely, if a cyst is not treated, a tumor may develop from its walls and a more serious surgical procedure may be required to remove it.
Despite the considerable concern regarding impacted third molars, a recent study sponsored by the American Association of Oral and Maxillofacial Surgeons and the Oral and Maxillofacial Surgery Foundation finds that third molars which have broken through the tissue and erupted into the mouth in a normal, upright position may be as prone to disease as those third molars that remain impacted.
Must the Tooth Come Out if it Hasn’t Caused Any Problems Yet?
Not all problems related to third molars are painful or visible. Damage can occur without your being aware of it.
As wisdom teeth grow, their roots become longer, the teeth become more difficult to remove and complications become more likely. In addition, impacted wisdom teeth are more likely to cause problems as patients age.
No one can predict when third molar complications will occur, but when they do, the circumstances can be much more painful and the teeth more difficult to treat. It is estimated that about 85% of third molars will eventually need to be removed.
When Should I Have My Wisdom Teeth Removed?
Wisdom teeth are easier to remove when the patient is younger, since their roots are not completely formed, the surrounding bone is softer, and there is less chance of damaging nearby nerves or other structures. Removal of wisdom teeth at a later age becomes more complicated as the roots have fully developed (may involve the nerve), and the jawbone is denser.
It isn’t wise to wait until your wisdom teeth start to bother you. In general, earlier removal of wisdom teeth results in a less complicated healing process.The AAOMS/OMSF study strongly recommends that wisdom teeth be removed by the time the patient is a young adult in order to prevent future problems and to ensure optimal healing.The researchers found that older patients may be at greater risk for disease, including periodontitis, in the tissues surrounding the third molars and adjacent teeth. Periodontal infections, such as those observed in this study, may affect your general health.
What Happens During Surgery?
Before surgery, your oral and maxillofacial surgeon will discuss with you what to expect. This is a good time to ask questions or express your concerns. It is especially important to let the doctor know about any illness you have and medications you are taking.
The relative ease with which a wisdom tooth may be removed depends on several conditions, including the position of the tooth and root development. Impacted wisdom teeth may require a more involved surgical procedure.
Most wisdom tooth extractions are performed in the oral and maxillofacial surgery office under local anesthesia, intravenous sedation or general anesthesia. Your oral and maxillofacial surgeon will discuss the anesthetic option that is right for you.
What Happens after Surgery?
Following surgery, you may experience some swelling and mild discomfort, which are part of the normal healing process. Cold compresses may help decrease the swelling, and medication prescribed by your Oral and Maxillofacial Surgeon can help manage the discomfort. You may be instructed to modify your diet following surgery and later progress to more normal foods.
Bone Grafting
What is a bone graft?
Bone grafting is the replacement or augmentation of the bone around the teeth.
Why is a bone graft needed?
Bone grafting is performed to reverse the bone loss / destruction caused by periodontal disease, trauma, or ill fitting removable dentures. It is also used to augment bone to permit implant placement, such as augmenting bone in the sinus area for implant placement, or augmenting bone to enhance the fit and comfort of removable prostheses, or to enhance esthetics of a missing tooth site in the smile zone. When one loses a tooth, as in an extraction, the surrounding bone collapses. To preserve this bone for future implant placement or for esthetics, a bone graft is used.
What are the types of bone graft?
1. autogenous – bone taken from one area of the patient and transplanted to another area requiring such grafting
2. allograft – either synthetic bone or bone from a bone bank (cadaver bone)
3. xenograft – bovine /cow bone
Which graft is used and when and why?
Autogenous bone is the “gold standard” and oftentimes has the most predictable results. This is described as the best type of graft because such bone is live bone with live active cellular elements that enhance bone growth, whereas other types of grafts are devoid of any active cellular material.
Allografts and Xenografts both do not require a second surgical site as does the autogenous bone. Ample amounts can be easily obtained.
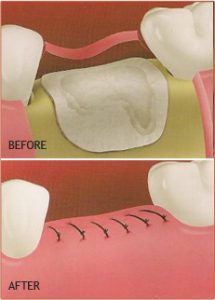
Barrier membranes – Guided Tissue Regeneration
In conjunction with bone grafting, membranes are often used to help stabilize the bone graft as well as displace the gum tissue from invading the healing bone graft. Gum tissue grows at a much faster rate than bone, therefore, membranes are used to prevent gum tissue from growing in and displacing the bone graft before it matures.
